___________
Cystatin C | National Kidney Foundation
Jul 26, 2023A past test for kidney function did not give clear results about your kidneys, so your healthcare provider wants to check again with a cystatin C test to be sure. You are older or have lots of muscle (such as a bodybuilder), where creatinine levels can vary. In these cases, a cystatin C test may
BLACK SEED OIL
4.2. Clinical Evidence of Kidney Protection by Black Cumin
Black cumin has shown improvement in disease outcomes in CKD patients as reported in several human studies. A recent systematic review and meta-analysis of randomized-controlled trials demonstrate that black cumin supplement in a long-term intervention and daily optimum dosage can significantly reduce parameters of kidney function, including BUN [85]. In a prospective, comparative, and open-labeled study on patients with CKD stages 3 and 4 at a tertiary care center in North India, treatment of NSO (2.5 mL, p.o., once daily for 12 weeks) significantly improved clinical features and biochemical parameters, including a reduction in blood urea, serum creatinine, and total urinary protein and an increase in total urine volume and glomerular filtration rate in 24 h [27]. Another similar study revealed the efficacy and safety of NSO administration in patients with CKD stages 3 and 4 due to diabetic nephropathy. There was a significant reduction in blood glucose, serum creatinine, blood urea, and 24 h total urinary protein levels and a significant increase in glomerular filtration rate, 24 h total urinary volume, and hemoglobin level in the group treated by black cumin oil [25]. In both studies, authors suggest that black cumin oil could be an add-on therapy that can boost the therapeutic advantage of conservative management in patients of diabetic nephropathy. Protection against nephrolithiasis as reported in preclinical study [
https://newhopeforkidneypatients.com/herbal-remedies-kidney-disease/
_____
Kidney stones & black seed oil:
Protection against nephrolithiasis as reported in preclinical study [71] was further translated into a randomized, triple-blind, placebo-controlled, clinical trial in which two groups of patients (each with 30) with renal stones received either black seed capsules (500 mg) or placebo twice daily for 10 weeks. In the black seed group, 44.4% of patients excreted their stones completely, and the size of the stones remained unchanged and decreased in 3.7% and 51.8% of patients, respectively, while in the placebo group, 15.3% of the patients excreted their stones completely, 11.5% had a reduction in stone size, 15.3% had an increase in stone size, and 57.6% had no change in their stone size. There was a significant difference in the mean size of renal stones between the two groups. Compared to placebo, black seeds have strong positive effects on the disappearance or reducing the size of kidney stones [26].
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8396533/
TMG (BETAINE)
_______
GINGER:
Ginger (Zingiber officinale Roscoe), a widely consumed medicinal plant, contains various bioactive phenolic compounds, including gingerols, shogaols, paradol, and Zingerone. These phenolic compounds have attracted research interest due to their diverse pharmacological properties. Emerging evidence suggests that these compounds hold renoprotective potential. This narrative review revisits the literature on the nephroprotective effects of ginger phenolics. Multiple studies conducted both in vitro settings and in vivo have shown that phenolic compounds found in ginger possess antioxidant, anti-inflammatory, antifibrotic, and kidney-protective properties in various models of kidney damage caused by drugs and metabolic diseases. Mechanistically, they modulate oxidative stress, inflammation, epithelial-mesenchymal transition, and apoptosis-related pathways. For example, gingerols and Zingerone reduced oxidative stress and improved kidney function in Cadmium- and cisplatin-induced nephrotoxicity models. Zingerone also exhibited renoprotection against vancomycin- and doxorubicin-induced kidney damage. Phenolic compounds found in ginger can also provide protection against kidney damage caused by renal ischemia/reperfusion and sepsis. Researches also indicate positive impacts in treating diabetic nephropathy and renal ischemia/reperfusion injury. The findings suggest that ginger phenolics could be effective in slowing down the progression of chronic kidney disease by targeting multiple aspects of kidney function. Yet, additional validation is needed to confirm their clinical significance. SOURCE:
https://www.sciencedirect.com/science/article/abs/pii/S2949824424002179
_______
RENAFOOD:
https://www.amazon.com/product-reviews/B071KD269Q/ref=acr_dpx_hist_5?ie=UTF8&filterByStar=five_star&reviewerType=all_reviews#reviews-filter-bar
________
Fenugreek supplements:
Fenugreek Supplement for Supporting Kidney Disease: In Vivo Studies
In vivo studies have demonstrated the potential benefits of fenugreek (Trigonella foenum-graecum) supplements in supporting kidney health, particularly in the context of nephrotoxicity induced by certain treatments.
Relevant Findings from In Vivo Research
- Study on Gentamicin-Induced Nephrotoxicity:
- A study investigated the effects of dried and germinated fenugreek seeds on kidney failure induced by gentamicin, an antibiotic known for its nephrotoxic effects.
- Male Swiss albino mice were utilized for this research, where they were divided into groups and received different treatments, including:
- Administration of gentamicin (100 mg/kg)
- Oral doses of dried and germinated fenugreek (500 mg/kg) for five days.
- The study evaluated several physiological parameters, including blood urea nitrogen (BUN), serum creatinine, and oxidative stress markers.
- Results:
- The administration of gentamicin significantly raised levels of BUN, serum creatinine, and oxidative stress indicators.
- Administering fenugreek, both in dried and germinated forms, showed ameliorative effects. It reduced oxidative stress markers and improved kidney function.
- Mechanisms of Action:
- Fenugreek is rich in antioxidants, particularly flavonoids and polyphenols, which contribute to its protective effects against oxidative damage.
- The study noted improvements in biochemical parameters, indicating that fenugreek could enhance renal function and mitigate oxidative stress.
Summary of Fenugreek’s Role
Fenugreek has shown promise as a supportive supplement for kidney health, particularly in scenarios of drug-induced nephrotoxicity. The antioxidant properties of its components may be key to its protective effects, making it a potential natural intervention in managing kidney health.
If you’re considering fenugreek as a supplement, it’s advisable to consult with a healthcare professional, especially in the context of existing kidney disease or other health conditions.
_______
Sepsis-induced acute kidney injury (SAKI) is one of the most frequent complications in patients with sepsis and is strongly associated with poor clinical outcomes. Trigonelline (TRL), a bioactive pyridine alkaloid isolated from fenugreek, has exhibited therapeutic effects on various diseases. This study aimed to investigate the effects of TRL on SAKI and whether TRL exerted its function via NAD+/SIRT1 pathway activation. A single dose (10 mg/kg body weight) of lipopolysaccharide (LPS) was intraperitoneally administered to establish a mouse SAKI model. After 24 h, compared with the control group, the plasma levels of kidney function indicators creatinine and blood urea nitrogen, oxidative stress indicators hydrogen peroxide and malondialdehyde, and inflammatory factors tumor necrosis factor-α and interleukin-1β were significantly increased. Meanwhile, hematoxylin and eosin staining results revealed that LPS treatment caused glomerular structure disruption, renal tubular luminal narrowing, and renal tubular structure deterioration. TRL treatment significantly reduced the plasma kidney function indicators, oxidative stress, and inflammatory factors levels in the SAKI mice, accompanied by improvements in the renal pathological changes. Furthermore, TRL treatment increased the NAD+ levels, upregulated the SIRT1 expression, and downregulated the NOX4 expression in the kidney of the SAKI mice. Subsequently, EX-527, a selective SIRT1 inhibitor, was used for inhibiting SIRT1, and it reversed the protective effect of TRL in SAKI. Our results revealed that TRL improved renal function and alleviated inflammation and oxidative stress in SAKI mice by NAD+/SIRT1 pathway activation. Therefore, TRL may be a potential therapeutic approach for SAKI treatment. SOURCE: https://www.researchgate.net/publication/393943791_Trigonelline_Attenuated_Sepsis-Induced_Acute_Kidney_Injury_by_Activating_NADSIRT1_Pathway
______________
CoQ-10 & kidneys:
Renal function is central maintaining health. Selenium and coenzyme Q10 are necessary to maintain normal cellular functions. As there is a documented deficiency of both substances in the elderly in many areas in the world, the effect of supplementation with selenium and coenzyme Q10 on renal function was evaluated.
Significantly better renal function in the active treatment group, as seen by evaluation of both creatinine and cystatin-C, could be reported. An estimation of glomerular filtration rated by use of CKD-EPI verified the positive effects. All evaluations were validated with persisting differences.
The obtained positive results could possibly be explained by effects on inflammation and oxidative stress by the intervention, but as the sample size was small, more research is needed. SOURCE:
https://pmc.ncbi.nlm.nih.gov/articles/PMC7764721/
https://healthunlocked.com/nkf-ckd/posts/151644109/excellent-article-on-importance-of-coq10-in-both-kidney-heart-function
XXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXXX
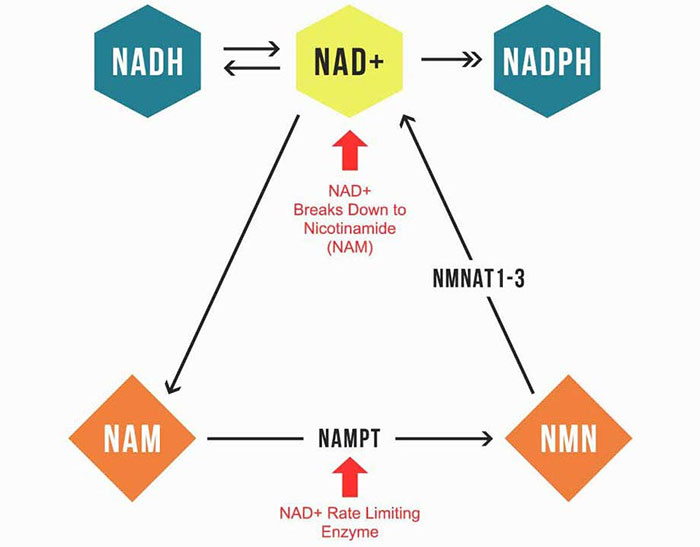
The reason I’m convinced niacinamide is the best NAD+ precursor is because the immediate breakdown product of NAD+ is niacinamide. As you can see in the illustration below, when NAD is used up, it gets broken down into niacinamide.
This niacinamide is then recycled. First, it’s converted into NMN, and then into NAD+. This is likely why some researchers promote NMN. However, the enzyme NMNAT1-3 that converts NMN to NAD+ is not the rate limiting enzyme. NAMPT is what controls how much NAD+ you make. So, flooding your body with NMN is not going to be as useful as using small amounts of niacinamide and activating NAMPT.
The ideal dosing of niacinamide is from 50 mg three times a day. It is the rare person that will not respond favorably to this simple intervention for increasing NAD+.
Niacinamide Prevents Kidney Disease
Speaking of NAD+, NAD+ deficiency has been linked to kidney disease, and niacinamide can help prevent that too.11 As Dinkov explains in a May 18, 2023, article:12
“Many studies have … shown that elevated lipolysis (delivering inflammatory PUFA to the kidneys) and, consequently, elevated fatty acid oxidation (FAO) as per the Randle Cycle are the … likely culprits. It is well-known that one of the effects of elevated FAO is a decline in the mitochondrial NAD/NADH ratio — i.e. relative deficiency of NAD+.
This is actually the primary mechanism through which elevated FAO inhibits glucose oxidation since lower NAD/NADH ratio inhibits the activity of the enzyme pyruvate dehydrogenase.
In any event, the study … demonstrates that relative deficiency in NAD+ (i.e. lower NAD/NADH ratio) is the direct cause of kidney damage due to the resulting OXPHOS dysfunction. Conversely, elevating NAD+ (and thus NAD/NADH) levels with precursors such as nicotinamide mononucleotide (NMN) or nicotinamide riboside (NR) was effective in completely preventing kidney damage and CKD.
Since NMN is no longer available over the counter and NR is rather expensive, niacinamide remains as the most viable option for replicating the study in humans with CKD, especially considering the fact that niacinamide is just as effective as an NAD+ precursor as NMN/NR while also having potential additional benefits the other two precursor do not.
Namely, niacinamide is an inhibitor of the NAD-consuming enzymes PARP-1 and CD38, so taking niacinamide not only directly increases NAD+ levels but also inhibits its excessive consumption/decline. I can’t find the actual published study that article is based on, but other studies have demonstrated benefits for CKD in animals from human-equivalent (HED) doses in the 250mg-500mg daily range.”
Reversing Chronic Kidney Disease with Niacin and Sodium Bicarbonate
Oct 14, 2021OMNS (Oct. 14, 2021) This story began with initial discovery, motivated by necessity. It would lead a few years later to reproducible documented reversal of chronic kidney disease (CKD) stages 1 or 2.
SOURCE:
FOR IMMEDIATE RELEASE
Orthomolecular Medicine News Service, October 14, 2021
Reversing Chronic Kidney Disease with Niacin and Sodium Bicarbonate
Review and Commentary by Stephen McConnell and W. Todd Penberthy
OMNS (Oct. 14, 2021) This story began with initial discovery, motivated by necessity. It would lead a few years later to reproducible documented reversal of chronic kidney disease (CKD) stages 1 or 2. Success was achieved using 3 to 5 cents/day of 100-500mg niacin TID [three times a day] along with 1.0-1.8 grams of sodium bicarbonate (baking soda, 600mg at lunch and 1.2g before bed) with or without < 2g/day elemental calcium, as calcium carbonate.
Excellent results from the use of niacin to treat CKD have now been documented for more than 25 case-studies. This approach is well supported by continuous basic and clinical research, including dozens of clinical trials that provide substantial evidence for the use of niacin and sodium bicarbonate. These approaches directly address the needs of the typical CKD patient. Unfortunately, this approach is rarely implemented in the clinical setting.
CKD commonly progresses with age as it is observed in 68% of Americans ≥ 60y of age. [1] Patients with CKD usually experience progressive loss of kidney function moving towards an increasing risk of end-stage renal disease (ESRD). CKD is the 9th leading cause of death in the US. [2] Fortunately, there are several simple approaches including the addition of modest doses of niacin (immediate release- or IR-Niacin) that can reverse CKD in many patients as described here.
Approximately 786,000 people per year, in the US progress to ESRD (stage 5 CKD), which is generally considered an irreversible condition. Most of these become completely dependent on regular trips to dialysis. Estimation of the stages of CKD is based on (GFR) glomerular filtration rates starting with ≤ 60mL/1.7m2 for 3mos as definitive of initial CKD diagnosis. Unfortunately, a creatinine derived GFR (crGFR) is only as reliable as the serum creatinine measure. Use of this creatinine-based test has a “blind-area” in the earlier stages, and frequently leads to an under-estimation of the true risk.
Stages of CKD
- Mild kidney damage, eGFR 90 or higher
- Mild loss of kidney function, eGFR 60-89
- Moderate loss of kidney function
- eGFR 45-59
- eGFR 30-44
- Severe loss of kidney function, eGFR 15-29
- Kidney failure or close to failure, eGFR less than 15
Niacin for CKD
Supplementation with daily low-dose niacin reliably reverses a large amount of the functional loss. This simple treatment is effective and critically important. Mortality rates with CKD are striking, as the 5-year survival rate for patients doing long-term dialysis is 35% compared to 25% in those with diabetes [T2DM] in the USA. [3]
Routinely, the first treatment approaches utilized for CKD patients, in the later stages, generally targets control of dysglycemia & reduction of hyperphosphatemia according to KDIGO guidelines. [4] Fortunately, there is an ever-increasing abundance of data revealing that simple niacin treatment is a profoundly effective treatment for reducing hyperphosphatemia — and that is just the beginning. In basic research the evidence in favor of niacin for CKD has continuously accumulated. Clinical research proves that the niacin stimulated pathways involving increased NAD synthesis, PCSK9 inhibition, sodium transporter effects, PPAR gamma activation, and more, are exceptionally well-suited to addressing CKD, multimorbidity, and ultimately all-cause mortality. [5-41]
The clinical and financial impact of CKD when it progresses to end-stage renal disease (dialysis-dependence; ESRD) is profound. Clinically, CKD progression quickly leads to lifelong dialysis with co-morbid life-threatening cardiovascular disease. Financially, The out-of-pocket cost of CKD is greater than cancer and stroke with ESRD dialysis costing 30.9 billion per year 2013 or approximately 7.1% of total Medicare costs. [42] Medicare spends approximately $250,000/y for every CKD patient, prior to the transition to ESRD and dialysis. Annual costs per dialysis patient can range from $720k to $2.2m per year. [43] These problems and their associated costs can be reduced by using 5 cents per day of niacin.
Originally, I (SM) was formally trained to operate a heart-lung machine, maintain full life-support & anesthesia, in the operating room monitoring patients undergoing open-heart surgery. Much later, I transitioned to working as a field scientist, MSL (Medical Science Liaison) in the advanced laboratory diagnostics industry. My primary clinical focus since that time has mainly been lipidology. Because of my initial education/training, addressing cardiovascular disease, I now focus on prevention: lipidology. This training gave me an appreciation for nicotinic acid (niacin, vitamin B3).
I have now personally observed more than 25 documented cases of individuals having their CKD progression not only halted but reversed with the addition of 3 to 5 cents worth of niacin, per day (with 1.8-2.4g/day sodium-bicarbonate with/without 250-500mg/day calcium-carbonate).
A family story
While I (SM) was learning lipidology in the period between 2002-2007, my father suddenly went to the ER late one Sunday night and my mother called me hysterically, “I took your father to the ER and now they are scheduling him for placement of stents.” I was concerned, as any son would be, but also as a scientist because I felt I may have ‘failed him,’ somehow: If only what I had already learned, I had only learned it, sooner.
My father was 81 at the time and he had been jumping rope for 30-minutes, twice daily. His body had a deceptively healthy look, and his triglycerides were low, but when we put it all together, he was “Pattern-B” — insulin resistant. He had always been a ‘stodgy,’ stubborn, stoic World War II veteran. He was very introverted and typically had a limited range of emotions: rage, laughter, and silence. Later, I would find out he had Asperger’s.
When I received the advanced laboratory data, it showed that he had low HDL2 and high ApoB. This is far more specific & confers much greater risk vs. an elevated LDL-C. Most importantly, this revealed he was insulin resistant a.k.a. pre-diabetic. At the time, I really didn’t fully understand this. Even today, most clinicians really do not, due to continued reliance on using only tests for FBG & HbA1c. Ultimately, my father survived that, and we continued to institute aggressive medical management: A hard lesson learned.
My father and my mother traveled everywhere together. They commuted, seasonally to Florida each winter, to escape the cold weather in Northwest Pennsylvania. On New Year’s Day, about 6 months after his MI & stent-placement procedure, I received a call from my mother, “Your father is in the hospital! They’re going to have to do open heart surgery!”
They needed to do an aortic-annuloplasty (aortic heart valve repair), in addition to a quintuple CABG (5 bypass grafts). I thought to myself, “this is getting worse and worse.” Having had previous personal experience working with thoracic surgeons during open-heart operations, I didn’t want the procedure to begin until my brother and I were able to be present. Fortunately, the young thoracic surgeon and the techniques planned were excellent.
Later, in the spring, they returned home to Erie, Pennsylvania for the follow-up visit. Dr. Dave (the physician who asked me to set-up my 1st lipid clinic) said, “Hey I got some bad news for you. Your dad has renal insufficiency.” I said, “Oh my God, he’s in renal failure, what stage is he?” He did not know. That was a flag. Most clinicians don’t know what stage their CKD patients are because the lab doesn’t do calculations and the creatinine measure is not reliable or accurate. The creatinine measure has very little accuracy until after the CKD has ‘hit’ stage 3B, and beyond. [44,45] So, a lot of these patients along the CKD disease continuum, through each progressive stage, appearing to have less risk vs. the ‘true’ risk that is present. It’s better to test a urine sample and see how much protein is recovered, and run a Cystatin-C and a crGFR to calculate a more accurate value. At that time, I only knew he was in failure, but when I did the crGFR calculation, I could see that he was well into the latter portion, of CKD-stage 4.
Recently, I had been putting together a new treatment algorithm with substantial literature support, data, on CKD. I was lucky to have been mentored by Dr. William F. Finn. [46]. Even if a patient has not already been scheduled for dialysis, he explained, and especially if they are currently on dialysis, you must get the serum phosphorus down. Excessive phosphorous is toxic to the kidneys as well as virtually every organ system and the entire body. [47,48] Phosphorus is a primary initiator of vascular calcification, among several other pathologies. If the kidneys start to lose a certain fraction of their normal function, the body can no longer efficiently clear phosphorous. When phosphorous serum levels reach abnormal levels, then you begin to saturate the tissues. Then phosphorous binds to calcium and it’s the phosphorous, not the calcium that starts the pathology leading to calcium phosphate stones.
Niacin helps to get the phosphorous down.
Even after you bring serum phosphate down you still have it in the tissues. The only biomarker available in a clinical setting, Fibroblast Growth Factor-23 (FGF-23), reflects the pathology behind long-term exposure to elevated phosphorus. FGF-23 can be decreased, simply by administering niacin. [14] However, the sodium phosphorous transporter works through a feedback mechanism to make more receptors to compensate.
So, calcium carbonate (from an antacid tablet) is commonly used first to bind the readily available intestinal phosphorous. This is among the cheapest and most effective phosphorus chelator approaches. Calcium carbonate should not be used above 2g/day elemental calcium, which is 40% of most of the formulations: Total 5g/day as calcium-carbonate. This should be administered at mealtime. The idea is to ‘treat the meal’, as there is generally very little phosphorous available to bind, outside of mealtime. When the kidney is in ‘failure’, after meals, excess phosphorous remains uncleared and leads to deposition in the tissues: valve leaflets; at the endothelial barrier; arterial subendothelial space (Mönckeberg’s medial calcification: arteriosclerosis). [49] When sodium bicarbonate (baking soda) is administered, based on the landmark study, [50,51] the transition from stages-3 & 4 to Stage-5/ESRD/Dialysis, can be reduced by ~80%, with just 1.8 grams sodium bicarbonate, alone. Mealtime dosing BID, (1X 600mg at lunch & 2X 600mg at dinner each day, i.e 1.8g total per day), optimizes the therapy.
In that study, the fraction of people of people that went to dialysis by the end of two years was roughly 35% on placebo, but the fraction that went to dialysis with the modest dose of sodium bicarbonate, was reduced roughly > 80%. [50] However, the concerns about sodium intake are frequently expressed. The literature is quite clear on this. The chloride salt of sodium is the issue, not the bicarbonate salt of sodium. This a key point. We just need to do a better job of identifying them early on. Do not assume the patient is stage 1 or 2 if the creatinine indicated that. We need better, more reliable biomarkers (EXAMP: Cystatin-C) and should insist the insurance companies reimburse for it.
This approach worked amazingly well for my father, because he reversed his CKD, by more than two stages! I calculated it incrementally based on where he was at each stage. He was nearing end-stage renal disease (stage 5) and he reverted back to stage 2, which was a virtual miracle at that time! I had never heard or seen of anything similar.
Niacin interested me when I came across a company that was working on a new chelator for phosphorus. I had already seen some literature on an extended-release niacin (ER-niacin) study showing a phosphorus-lowering effect and IR-Niacin having an antiproteinuric effect. Niacin was so effective that it moved the GFR up enough to reverse the baseline status by a full stage, even at very low doses. This seemed to be the plausible explanation for this net result.
Niacin (as well as no-flush niacinamide/nicotinamide) inhibits the sodium phosphate transporter. There are at least twenty peer-reviewed publications demonstrating this. [5-41,52-59] What was discovered was, if you want to control phosphorus, niacin is one the most effective methods and its efficacy is not affected by timing relative to meals. As little as 100mg of niacin will effectively reduce the serum phosphorus.
Some studies refer to this niacin-mediated effect as the “phosphorous fix”. The additional CKD benefits of niacin include the antiproteinuric, as well. If you compare a blood test vs. urine test, then the urine is probably a much more reliable indicator, because when the basement membrane is damaged, filtration is impaired such that the basement membrane between the podocyte processes no longer conserves plasma proteins & the amount lost, ‘leaked’ is present in the urine. The appearance of albumin (protein) in the urine is a ‘flag’ that loss of serum protein due to impaired renal function. Often, this is one of the earliest markers. Blood biomarkers have some variables that could result in misclassification of CKD stages. Protein leaking from the kidneys, is a direct correlate to the podocyte/basement-membrane damage. This is the gold-standard measure of endothelial function. I always like to use at least one blood marker (ideally CystatinC) in addition to the urine test, to facilitate extrapolating, “pinpointing” the true stage at baseline and where they are at follow-up.
I believe niacin is probably one of the best treatment options for a variety of chronic conditions/pathologies. CKD is a complex disease state. At its ‘core’, it is a vascular disease, but If you “hit all the right buttons” it is clearly possible to ‘drive’ CKD backwards.
With stage-5-CKD a.k.a. end-stage renal disease (ESRD), the scarcity of donor organs is a primary challenge. The reality is usually that dialysis will be required for the rest of the patient’s life. That is a powerful motivator to the patient to consider niacin.
Ultimately my father’s CKD, reversed from stage 4 to stage 2. When the sum of all the data, connecting-the-dots with all the biomarkers, he was close to end stage renal disease as he was scheduled to have a 1st encounter with a nephrologist. So, he was likely headed to dialysis, sooner vs. later.
The Current State of CKD Treatment & the Importance of Addressing Multimorbidity
In regard to prevention, many physicians choose not to believe there is any way to prevent or reverse CKD. Unfortunately, most patients end up on dialysis, or at the very least their CKD continues to get worse.
Too often, a less than adequate job of correctly identifying pre-diabetes is implemented, early on in the CKD disease state. It is vitally important to have a method of measuring the glucose post-prandial (PPG) level at 1h and 2h post-glucose challenge (OGTT). Currently, this is the gold standard test for assessing pre-diabetes. There are blood biomarkers that have a VERY high level of precision determining the 1-hr PPG: 1,5-AG & AHB (Alpha-HydroxyButyrate).
Measures of fasting insulin, fasting glucose, and HbA1c can miss an unacceptably large number of pre-diabetics. The OGTT test, will reliably capture a pre-diabetes diagnosis. HOMA-IR (HOMA-IR; homeostasis model assessment as an index of insulin resistance) is an effective method to calculate and evaluate insulin resistance using conventional reference lab biomarkers: insulin levels, fasting glucose levels, and A1C [60,61]. If you have these 3, you can then calculate the HOMA-IR. This enables accurate documentation and validates spending the modest expense to do the proper tests.
As much as 70% of adults over the age of 30 do not have normal postprandial glucose (PPG). It’s that bad! They say it’s only 30% or 40%, but that’s likely based on poor statistics. In fact, during every year in the last several decades, the percentage of individuals over the age of 30 with obesity has risen. The antiquated Frederickson classification was based on cholesterol/triglyceride parameters, but we are presently in the ‘particle age’ of clinical lipidemia assessment. Like the Frederickson classification for lipid disorder sub-types (which was largely based on cholesterol measurements), current methods to assess the presence & severity of insulin-resistance a.k.a. pre-diabetes, are essentially obsolete.
Another aspect to consider is multiple comorbidities. Modern medicine currently generally takes the approach of treating one condition at a time, but there are nearly always multiple disease symptoms present that are tightly associated and anything that can ultimately address this is going to result in the most effective therapies, ideally prior to the fulminant disease.
The Academy of Medical Sciences declared in 2018 that multimorbidity is the number one top priority in healthcare research. [62] Estimates for a cure of cancer reveal that this would only increase lifespan by a mere 3 years on average because the associated co-morbidities were not addressed. [63] Niacin, however, addresses so many common denominators for disparate diseases that the impact of niacin treatment for CKD/ESRD is likely to benefit many more indications, especially the number one killer, cardiovascular disease.
At the end of the day, it is the effect on all-cause mortality that matters the most for any treatment. After the termination of the Coronary Drug Project-CDP trial, it was determined that all-cause mortality was reduced by 11%, 9 years after stopping niacin treatment (avg. dose 2.4 g/day). [64] This may be a feat an unparalleled in proven clinical medicine. By contrast, statin all-cause mortality data has yielded mixed results.
Conclusion
In over 25 documented individual cases of CKD stages 2 through 4, after initiation of a combination-therapy of supplements based on GFR, including 500mg TID IR-Niacin, over a 3-month period, it was possible to improve their disease by at least one stage.
In basic and clinical research the evidence in favor of niacin for CKD is strong. Clinical research proves that the niacin is exceptionally well-suited to treatment and prevention of CKD, multimorbidity, and ultimately all-cause mortality.
Sampathkumar explained the current CKD treatment with niacin situation best, “Pharmaceutical industry driven large-scale studies are unlikely to be undertaken given the low-cost of niacin. David is up against the formidable Goliath of players promoting costly non-calcium containing phosphorus binders. It is time that international bodies like Kidney Disease, Improving Global Outcomes (KDIGO) take a call on usefulness of niacin as a low-cost, effective, and low pill burden agent for phosphorus reduction in CKD with multiple pleotropic benefits.” [29]
Recommended Doses to address Chronic Kidney Disease
Low-dose immediate release-niacin, 100mg – 500 mg, 1 to 3x/day. No-flush niacin or niacinamide will have equal efficacy on lowering phosphorus levels, but negligible cardio-vascular benefits compared with standard niacin.
Sodium Bicarbonate (baking soda) 1.8g/d (1/3 at lunch and 2/3 at dinner).
Calcium carbonate antacid pills (400-1000mg elemental calcium or 2-4gms antacid tablets) with food to bind phosphorous in food.
Low-Dose-Thyroid Supplementation| (25-50µg T4/Levothyroxine or 1/2grain of Desiccated Thyroid).
Methyl Folate (0.8g to 2mg L-MethylFolate).
Recommended Additional Monitoring
A full panel of metabolic parameters [baseline & 90-day f/u] can also determine ‘collateral’ benefit[s], especially related to cardiovascular health:
Apo-B decreases
Apo-A1 increases (INTERHEART Study)
Lp(a) mass decreases
Lp-PLA2 decreases
MPO/myeloperoxidase| decreases
AST/ALT/GGT hepatic parameters improved
Symptomology/Signs-Symptoms: TIA; Chronic Angina; Claudication; Dyspnea upon Exertion.
The views of the authors, who are not physicians, are presented here for educational purposes. All readers are reminded to be sure to work with their own health care provider(s) before commencing this or any nutrition-based approach.
(Stephen D. McConnell is a lipidemiologist and researcher with an MSc in Cardiovascular and Renal Pathophysiology. W. Todd Penberthy, PhD, specializes in writing about targeted pharmacotherapeutics, CME, and biomedical texts.)
References
1. Kidney Disease Statistics for the United States. NIDDK. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/health-statistics/kidney-disease
2. National Center for Health Statistics (2021) Deaths and Mortality. FastStats. https://www.cdc.gov/nchs/fastats/deaths.htm.
3. US Renal Data System. (2018) Chapter 1: Incidence, Prevalence, Patient Characteristics, and Treatment Modalities. 2:291-331. https://www.usrds.org/media/1736/v2_c01_incprev_18_usrds.pdf
58. Ilkhani F, Hosseini B, Saedisomeolia A (2016) Niacin and Oxidative Stress: A Mini-Review. J Nutri Med Diet Care. 2:014. https://clinmedjournals.org/articles/jnmdc/journal-of-nutritional-medicine-and-diet-care-jnmdc-2-014.php
59. Lenglet A, Liabeuf S, Guffroy P, et al. (2013) Use of Nicotinamide to Treat Hyperphosphatemia in Dialysis Patients. Drugs R D 13:165-173. https://pubmed.ncbi.nlm.nih.gov/24000048
60. Matthews DR, Hosker JP, Rudenski AS, et al. (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia, 28:412-419. https://pubmed.ncbi.nlm.nih.gov/3899825
61. Wallace TM, Levy JC, Matthews DR (2004) Use and abuse of HOMA modeling Diabetes Care 27:1487-1495. https://pubmed.ncbi.nlm.nih.gov/15161807
62. Editorial (2018) Making more of multimorbidity: an emerging priority. The Lancet. 391:1637 https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(18)30941-3/fulltext.
63. Arias E, Heron M, Tejada-Vera B. (2013) United States life tables eliminating certain causes of death, 1999-2001. Natl Vital Stat Rep 61:1-128. https://pubmed.ncbi.nlm.nih.gov/24968617
64. Canner PL, Berge KG, Wenger NK, et al. (1986) Fifteen year mortality in Coronary Drug Project patients: long-term benefit with niacin. J Am Coll Cardiol 8:1245-1255. https://pubmed.ncbi.nlm.nih.gov/3782631
Nutritional Medicine is Orthomolecular Medicine
Orthomolecular medicine uses safe, effective nutritional therapy to fight illness. For more information: http://www.orthomolecular.org
To Subscribe at no charge: http://www.orthomolecular.org/subscribe.html
To Unsubscribe from this list: http://www.orthomolecular.org/unsubscribe.html
Western medicine do not understand the kidneys like Chinese doctors do. Western doctors known that the kidneys are responsible for fluid balance, waste elimination, regulation of blood pH and mineral balance. They also play an important role in red blood cell production, blood pressure regulation and converting vitamin D to its active form, calcitriol. Our kidneys are essential for life.
The worst part about living with kidney disease is that it is a silent killer. However, what makes it more dangerous is the fact that it usually is only recognized at extremely late stages when it is extremely difficult to treat.
Signs and Symptoms
The first symptom of kidney disease is a change in the amount and frequency of the urine you pass. There may be increase or decrease in amount of urine you pass and dark colored urine (darker than usual). According to Dr Avinash Ignatius, senior consultant nephrologist DaVita, Pune Region, “Frequent urination at night is one of the most common and early symptom of chronic kidney disease and it should not be ignored even though it appears to be harmless. Other symptoms of the disease usually develop at later stage when the kidneys have lost approximately 80% of its function.’
Other symptoms include difficulty or pain while urinating, blood in the urine, foamy urine, swelling or edema, extreme fatigue, anemia and generalized weakness, dizziness, and inability to concentrate. Feeling cold all the time, cold back, cold hands and feet are also a common and primary symptom of kidney disease.
Shortness of breath is another common symptom because of kidney disease. When severe enough a build-up of fluid in the lungs, or because of anemia (a common side effect of kidney disease), starves your body of oxygen making you suffer from breathlessness. Another explanation and cause of kidney disease is fast shallow breathing (as opposed to abdominal breathing), which does not allow the energy and oxygen to reach down to touch the kidneys.
A major sign of kidney disease is severe pain in the back or sides. This is a common indicator of kidney disease but is not seen in everyone who suffers from the condition. The pain is characteristic and you may feel a severe cramping pain that spreads from the lower back into the groin.
Inherent kidney energy may be low from birth is progressively depleted with age. It is particularly vulnerable to exhaustion due to factors such as overwork, a hard-driven lifestyle, insufficient fluid intake, multiple pregnancies, and chronic illness or stress.
For most people by the age of 40, declining Kidney energy is beginning to impact on their health. Unchecked, it can manifest as infertility, sexual dysfunction, menopause, andropause, prostate problems, impaired immunity, chronic inflammation, high blood pressure, heart irregularities, anxiety, loss of physical drive and poor concentration.
Other signs and symptoms that your Kidneys are depleted include a sore or weak low back, knees, or ankles; bone or tooth problems; dark circles under your eyes; hearing problems; and premature graying or thinning of your hair. Thyroid problems or extreme reactions to the climate—feeling really cold or having lots of hot flashes—are also indications that your Kidney is out of balance. Edema, kidney stones, and getting up several times each night to urinate suggest a problem with the water metabolism function of the Kidney and Urinary Bladder.
The functionality of the Kidneys
Western physiology and anatomy limit its description of the kidney to the actual organ itself, whereas Chinese medicine sees and defines the kidneys not just as an organ but a group of functions, as well as being the root of energy for the entire body. The emphasis of Chinese physiological theory is more in terms of function rather than form.
In Chinese medicine, the Kidney (with a capital ‘K’ to denote the organ-meridian system) is important as it is the source of the body’s constitutional or inherited energy and is regarded as the organ-meridian system that governs the structural integrity and function not only of the kidneys themselves but also the adrenal glands, ovaries, testes, brain, spinal cord, skeletal structure (especially the lumbar region), teeth, anus, urethra and inner ear. The Kidney system also governs hormones and other substances produced by the kidneys, adrenals and sex glands, as well as reproduction, growth and the faculty of will power.
Dehydration and Kidney Disease
Thus under normal circumstances, many of us flirt with mild dehydration over sustained periods. Shortness of breath is a common symptom of dehydration and so is low energy. When someone is dehydrated and experiencing these symptoms one merely has to drink several glasses of water to fuel the body’s an almost instant response to hydration. Add some sodium bicarbonate and the response is even greater.

Courtesy of Brian D. Foltz
It makes perfect sense that chronic dehydration would be a problem for the kidneys. The element in nature associated with the Kidney is water, which is appropriate and symbolic in that water is the source of all life. The organ paired with the Kidney is the Urinary Bladder, and together both organs govern water metabolism in the body.
Sexuality and creativity are emotional components of the Kidney system. As the organ that governs survival through reproduction, the Kidney system is responsible for libido and strength of sexual attraction.
The emotions associated with kidneys are fear and fright. Fear has the ability to shake you to your core, and chronic fright translates into something very much like unrelenting stress, which is extremely damaging to the Kidney. In Western medicine, your adrenal glands pump out adrenaline (stress hormones) and are located right next to your Kidneys.
For the rest of this great read by doctor Sircus please use this link:
http://drsircus.com/kidney-disease/natural-treatments-reverse-kidney-disease/
Natural Remedies for Kidney Disease:
https://pubmed.ncbi.nlm.nih.gov/32481844/

_____
https://nephcure.org/wp-content/uploads/2019/01/Natural-Medicine-Kidney-Disease.pdf
cordyceps, melatonin, gingko biloba, Rutin, & Fo-ti mentioned above link
_____
https://pubmed.ncbi.nlm.nih.gov/35988461/
https://www.sciencedirect.com/topics/medicine-and-dentistry/rhubarb-extract
http://healingtools.tripod.com/thn5.html
https://www.curezone.org/forums/am.asp?i=1216769
https://www.ncbi.nlm.nih.gov/pubmed/23134313
https://www.ncbi.nlm.nih.gov/pubmed/23360312
https://www.sciencedaily.com/releases/2017/12/171207141711.htm
https://www.ncbi.nlm.nih.gov/books/NBK92775/
Supplements:
http://www.lifeextension.com/Magazine/2010/5/Innovative-Strategies-to-Combat-Kidney-Disease/Page-01
https://paulhaider.wordpress.com/2015/12/01/bentonite-clay-for-kidney-disease-gi-tract-and-detoxing/
https://www.naturalhealth365.com/0959_kidney_disease_clay/
https://www.globalhealingcenter.com/natural-health/7-best-foods-support-kidney-function/
https://www.sciencedaily.com/releases/2014/01/140115075624.htm
Baking soda ***
https://www.sciencedaily.com/releases/2018/04/180425093745.htm
https://www.healthy-holistic-living.com/drinking-baking-soda-inexpensive-safe-way-combat-autoimmune-disease-study/?utm_source=DM&fbclid=IwAR0RzTjAeQmdwLmL66SeFHWLbCWQQxv4Yf6Mo6dKrmp8WQq7u9s8GHeFp3Y
https://www.eurekalert.org/pub_releases/2018-04/mcog-dbs042418.php
https://www.bestremedies.net/7-best-herbs-supplements-kidneys-includes-kidney-tonic-soup-recipe-steps-kidney-cleanse/
https://drcarolyndean.com/2013/09/kidneys-need-magnesium-2/
https://www.cherylsherbs.com/home/herbal-profile-nettle-leaf-root-seed/
Studies: *** If a link says no info, highlight it & hit go to Https:……..
https://brioclinic.com/blogs/products/14445793-cordyceps-kidney-and-renal-benefits
http://www.life-enhancement.com/magazine/article/3166-mechanisms-of-taurine-in-the-kidneys
Bentonite Clay:
https://www.naturalhealth365.com/0959_kidney_disease_clay/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4224708/
http://aminoacidinformation.com/taurine-amino-acid-kidney-disease/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3634170/
https://www.ncbi.nlm.nih.gov/pubmed/28178874
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4297707/
https://www.ncbi.nlm.nih.gov/pubmed/25474287?fbclid=IwAR19x3JPfHsq89FGtbnUI-hEjxOFUwXo-BFdFEMFeVVEAu79gWLK4FgwQ6U
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4389982/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5632318/
http://onlinelibrary.wiley.com/doi/10.1002/dat.20594/full
https://www.ncbi.nlm.nih.gov/pubmed/14713855
https://www.ncbi.nlm.nih.gov/pubmed/23828329
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5412196/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4884213/
https://www.ncbi.nlm.nih.gov/pubmed/20041816
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3249924/
http://www.lifeextension.com/Magazine/2011/6/Proprietary-Green-Tea-Extract-Protects-the-Kidneys/Page-01
One woman’s fight for her father’s kidneys:
http://kaveri.org/wp/2006/11/kidney-therapy/
These components found here in galangal:
Galangal is a low calorie, a low-fat rhizome that is extremely good for your health. A serving of this herb is found to contain about 2 g of dietary fiber and 45 calories. It also contains vitamins A, vitamin C and minerals like sodium and iron. It is also a good source of phytochemicals including galangin, alpinin, emodin, kaemperol, kaempferide, quercetin, and beta-Sitosterol. These flavonoids constitute most of the medicinal properties of galangal.
( are TRPC5 inhibitors)
Source: https://www.sciencedaily.com/releases/2017/12/171207141711.htm
https://www.ncbi.nlm.nih.gov/pubmed/26565375
Please watch it at min. 37:35 – 38 below:


PLEASE BOOKMARK MY BLOG & SHARE IT.